Cervical cancer is the fourth most frequent cancer in women worldwide, representing nearly 8 per cent of all female cancer deaths every year.
Of the estimated incidence and mortality from cervical cancer, approximately 84 per cent of all cases and 88 per cent of all deaths occurred in low- and middleincome countries (world health organization, WHO).
Persistent high-risk human papilloma virus (hrHPV) infection is the primary cause for cervical cancer.
Periodic surveillance through hrHPV and Pap smearbased testing has remarkably reduced cervical cancer incidence worldwide.
However, it is a sad fact that despite being almost completely preventable through human papillomavirus (HPV) vaccination and screening, cervical cancer remains largely uncontrolled in high-risk developing countries primarily due to ineffective or no screening program.
Nine out of ten women who die from cervical cancer live in low- and middle-income countries.
Treatment approaches and outcomes for cervical cancer patients are highly dependent on disease stage at diagnosis.
Cervical cancer: global scenario
Global cancer burden using the global cancer observatory (GLOBOCAN) 2020 estimates of cervical cancer incidence and mortality produced by the International Agency for Research on Cancer (IARC) across the globe in 2020, there were an estimated 604,127 cervical cancer cases and 341,831 deaths, with a corresponding age-standardized incidence of 13·3 cases per 100,000 women-years and mortality rate of 7·2 deaths per 100,000 women-years. Cervical cancer incidence ranged from 2·2 in Iraq to 84·6 in Eswatini, and mortality rates ranged from 1·0 in Switzerland to 55·7 in Eswatini (Lancet Glob Health Vol 11 Feb 2023). WHO launched the Global Cervical Cancer Elimination Initiative to accelerate the elimination of cervical cancer, aiming to reduce incidence below a threshold of 4 cases per 100,000 women-years in every country and thus narrow international disparities associated with this disease.
Cervical cancer in Fiji
The top five most common cancers, in order of frequency (excluding non-melanoma skin cancers), among women in Fiji include breast, cervix, uterus, thyroid and ovary. Fiji has a population of 314,337 women between the ages of 15 years and older who are at risk of developing cervical cancer. In Fiji, crude cervical cancer incidence per 100,000 women was 30.7, the age-standardized incidence of cervical cancer was 29.8 and the mortality rate was 20.7 (GLOBOCAN 2020). Current estimates indicate that every year 136 women are diagnosed with cervical cancer and 92 die from the disease. Cervical cancer ranks as the second most frequent cancer among women in Fiji and the second most frequent cancer among women between 15 and 44 years of age. Though, the exact data is not available on the HPV burden in the general population of Fiji, in Melanesia, the region Fiji belongs to, about 7.7 per cent of women in the general population are estimated to harbour cervical HPV-16 or 18 infection at a given time, and 82.9 per cent of invasive cervical cancers are attributed to HPVs 16 or 18 (HPV information centre, Fiji, Fact sheet March 2023). Studies show that only 1 in 10 women screened for cervical cancer in the last 5 years (WHO – Cervical cancer profile Fiji 2021).
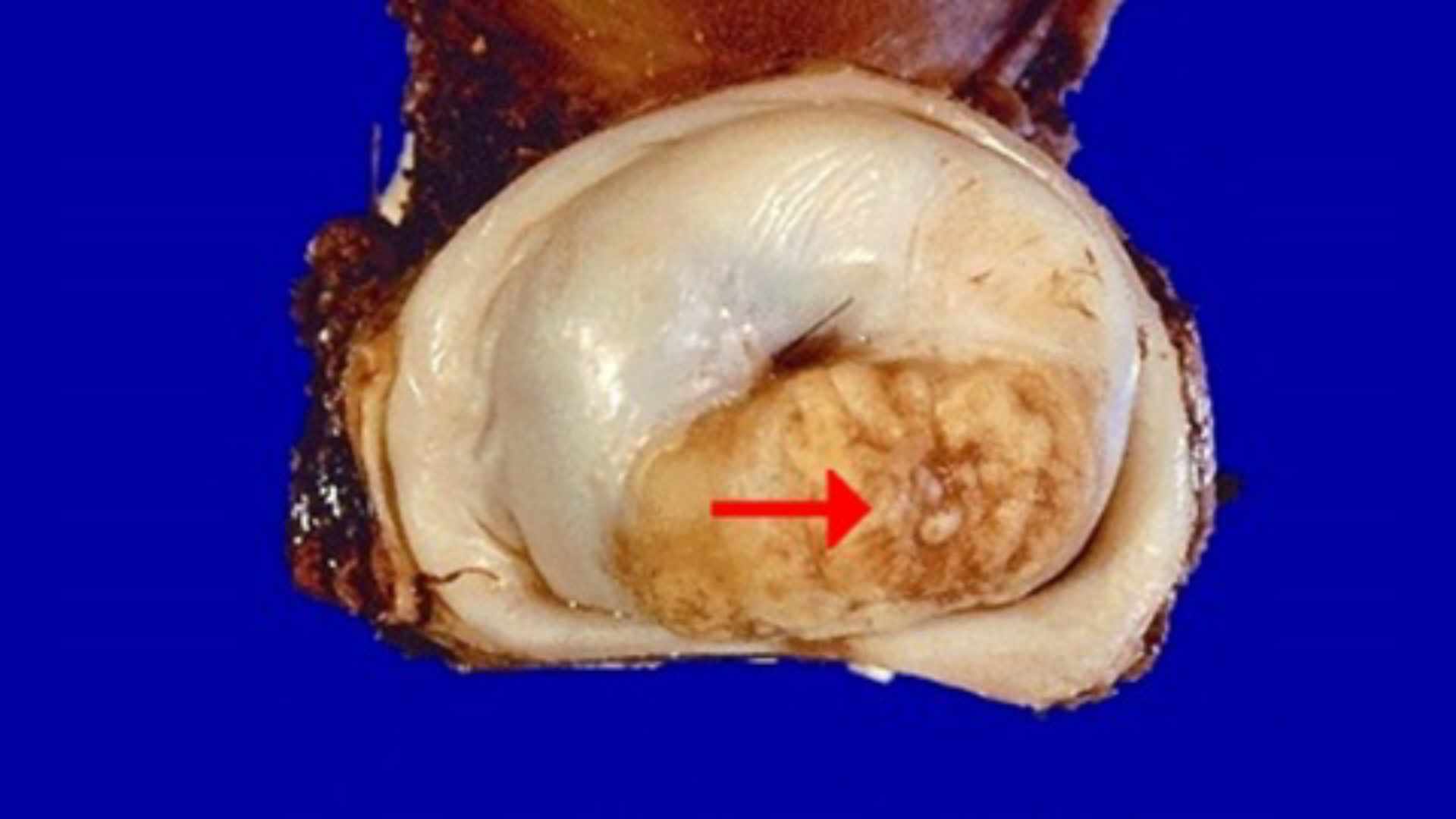
Human papilloma virus (HPV) and cervical cancer
Cervical cancer is by far the most common HPV-related disease. Epidemiological studies report that almost all cases of cervical cancer (more than 95 per cent) are caused by HPV. HPV is the most common viral infection of the reproductive tract and it is transmitted through close skin to skin contact, usually during sexual activity. Most sexually active women and men will be infected at some point in their lives, and some may be repeatedly infected. There are many different types of HPV. Most are harmless but some cause genital warts, and others cause changes that can develop into cancer. As well as cervical cancer, HPV can cause anal, vaginal, vulval, penile and some types of mouth and throat cancers. In general, most HPV infections (more than 90 per cent) clear up on their own and most pre-cancerous lesions resolve spontaneously. However, if it establishes a persistent infection with high-risk genotypes, such as HPV 16 and 18, there is a risk for all women that HPV infection may become chronic and there is high association with cervical cancer. Though around 12 types of HPV are considered high risk for cancer of the cervix, both of the HPV sub-types 16 and 18 jointly cause 70–75 per cent of all cervical cancers and 40–60 per cent of its precursor lesions. It takes 15 to 20 years for cervical cancer to develop in women with normal immune systems. But it can take only 5 to 10 years in women with weakened immune systems, such as those with untreated human immunodeficiency virus (HIV) infection. And the likelihood that a woman living with HIV will develop invasive cervical cancer is up to six times higher than for a woman who is not living with HIV.
Screening for cervical cancer: HPV DNA test and Pap smear test
Screening is testing of all women at risk of cervical cancer. Testing is done among women who have no symptoms and may feel perfectly healthy. Screening aims to detect precancerous changes, which, if not treated, may lead to cancer. Cervical cancer screening involves testing for HPV infection to detect pre-cancer and cancer, followed by treatment as appropriate. When screening detects an HPV infection or precancerous lesions, these can easily be treated and cancer can be avoided. Screening can also detect cancer at an early stage where treatment has a high potential for cure. HPV primary screening tests the cervical cells for the HPV virus first. The laboratory will look to see if high risk HPV is present. If high risk HPV is found, the laboratory will test the sample for cell changes (Pap smear cytology). However, in some parts of the world, they look for changes in the cervical cells first. They then test for HPV if there are cell changes. High risk HPV can cause cell changes in the cervix, which over time can develop into cancer. Not all cell changes will develop into cancer but it’s important to monitor any changes and give treatment if necessary. Studies showed that the CO- VID-19 pandemic has created a new group of susceptible women due to the decrease in screening intensity and detection of cervical precancers, but has also boosted the introduction of HPV testing of self-collected specimens, which offers possibilities to increase population coverage (WHO).
Pap smear test
Pap smear test denotes study of cervical cells for cellular changes caused by HPV, and it is a very important and useful method for cervical cancer screening. Globally, efforts to prevent the disease include screening women using Pap smears and treating precancerous lesions. Impressive results have been achieved in reducing cervical cancer incidence and mortality in some developed countries by Pap smear screening. Both HPV DNA test and Pap smear test are available at Oceania hospitals. Screening should start from 30 years of age in the general population of women, with regular screening with a validated HPV test every 5 to 10 years, and from 25 years of age for women living with HIV. And, women living with HIV also need to be screened more frequently, every 3 to 5 years (WHO). Cervical cancer incidence can be reduced by as much as 90 per cent where screening quality and coverage are high. However, in developing countries – where approximately 80 per cent of all new cases occur – many women have never had a Pap smear. Proper implementation of screening programs is essential to reduce the incidence and mortality of cervical cancer.
Conclusion
Cervical cancer is a global public health problem, with a particularly high burden in many lowincome and middle-income countries. It shows a clear socioeconomic gradient, with deceasing rates as human development index (HDI) increased. Incidence was three times higher in countries with low HDI than countries with very high HDI, whereas mortality rates were six times higher in low HDI countries versus very high HDI countries. Cervical cancer is one of the leading causes of cancer death among women in Fiji and Pacific Island countries. Presumably, the increase in cervical cancer cases in Fiji and other Pacific Island countries is a result of less women getting HPV and Pap smear test. Cervical cancer remains largely uncontrolled in high-risk developing countries because of ineffective or no screening program. The best way to find cervical cancer early is to have regular screening tests. The tests for cervical cancer screening are the HPV test and the Pap test. These tests can be done alone or at the same time (called a cotest). Regular screening has been shown to prevent cervical cancers and save lives. Proper implementation of screening programs is essential to reduce the incidence and mortality of cervical cancer. Cervical cancer can have devastating effects with a very high human, social and economic cost, affecting women in their prime. But this disease should not be a death sentence. I would like to conclude with the statement of Dr Tedros, Director-General, WHO “one woman dies of cervical cancer every two minutes. Each one is a tragedy, and we can prevent it”.
•DR SIVASELVAM SIVAKUMAR is the Head of Laboratory and Consultant Histopathologist and Cytopathologist, at Oceania Hospital Pte Ltd. He has held various positions in the medical fraternity across India, Malaysia, Saudi Arabia, and the UK. The views expressed in this article are his and do not necessarily reflect the views of this newspaper.