FIJI is grappling with a rising HIV epidemic that could reach catastrophic levels in the coming years if preventative measures are not put in place.
The Ministry of Health is sounding the alarm, warning that based on current trends, the number of HIV cases could soar to 20,000 within the next four years.
This projection comes after Health Ministry officials revealed alarming statistics and trends in HIV transmission, particularly among young adults and injecting drug users.
Health Minister Dr Atonio Lalabalavu recently declared an official HIV outbreak in the country, citing a significant surge in new cases and related deaths.
Between January and September 2024 alone, 1093 new HIV cases were recorded, along with 115 HIV-related deaths.
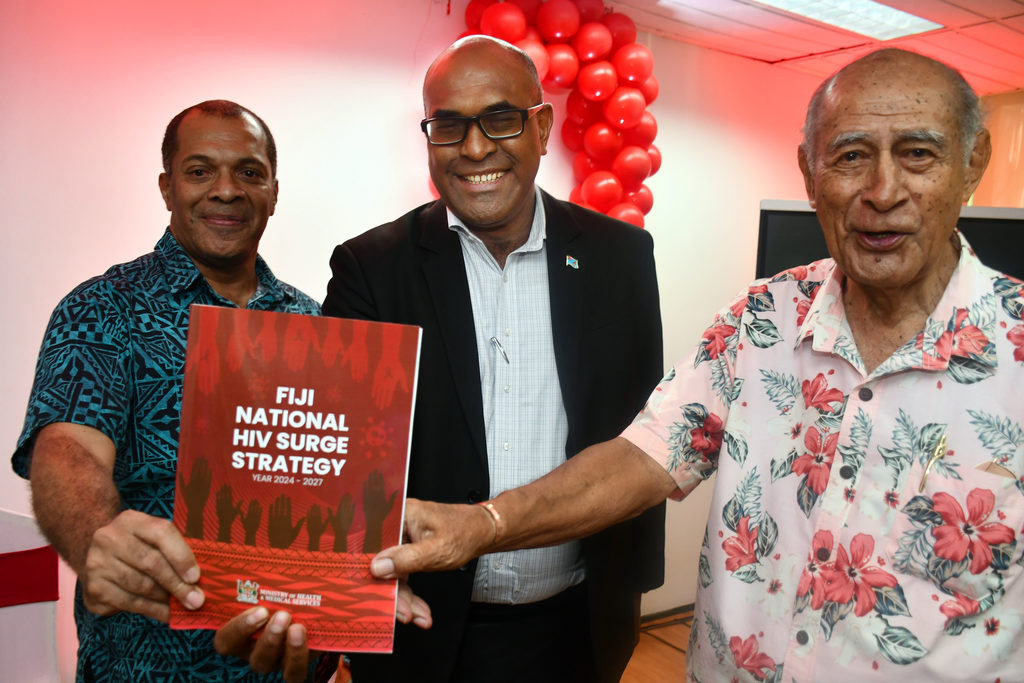
To address this national crisis, the Ministry launched the HIV Outbreak Response Plan and National HIV Surge Strategy 2024-2027 on Wednesday, January 22, 2025.
The permanent secretary for the Ministry of Health, Dr Jemesa Tudravu, provided an in-depth overview of the situation during the launch of the document.
“Over the last five years, the rate of reported HIV cases has increased ninefold, from 13.56 per 100,000 population in 2019 to 123.52 per 100,000 population in 2024,” Dr Tudravu said.
“We have also noted that 72 per cent of all our diagnosed cases in 2024 were in men.”
He said this increase was particularly evident in the Central and Eastern divisions, where injecting drug use has contributed to the vast majority of new cases.
Injecting drug use and its role in the surge
Injecting drug use has become one of the leading drivers of HIV transmission in Fiji, accounting for 55 per cent of new HIV cases in the country in 2023.
Dr Tudravu shared that the Western Division, with a similar pattern, reported that nearly half (48 percent) of HIV-positive individuals had contracted the virus through intravenous drug use.
“A person who injects drugs and shares used needles is 29 times more likely to contract HIV, and our data today is a clear reflection of this.
“This data underscores the urgent need for harm reduction strategies such as needle exchange programs and pre-exposure prophylaxis (PrEP), which have shown success in other high-prevalence countries.”
Dr Tudravu said without intervention, the number of people living with HIV could escalate dramatically.
Projections indicate that the HIV burden in Fiji could reach 25,000 cases by 2028, fueled by continued unsafe practices, including needle sharing among drug users.
“We need to consider and rapidly introduce high-impact prevention interventions that have been successful in high-prevalent countries.”
He said those figures had prompted the ministry to take bold steps to curb the spread of HIV and improve treatment access for those already living with the virus.
The challenge of treatment and follow-up
While the current estimate places the number of people living with HIV in Fiji at about 6100, the majority of these individuals are not receiving the necessary treatment.
Dr Tudravu said only 35 per cent of those living with HIV were currently on treatment, a significant gap that poses both health risks to individuals and public health concerns because of the potential for further transmission.
“That means they’ve been diagnosed, they’ve started treatment, and they’ve walked away and have not come back.
“They have not maintained their treatment. Untreated HIV individuals are at risk of serious health impacts, including death.
“And importantly, untreated people are able to transmit HIV to others.
“So treatment is a fundamental prevention tool.”
Dr Tudravu said the ministry was working to expand treatment access by increasing testing sites and opportunities for individuals at risk to get tested and connected to care.
The aim is to ensure that 95 per cent of all people living with HIV are on treatment, a goal that will require a substantial effort from both the ministry and international partners.
The HIV outbreak response Plan
In response to the crisis, the Ministry of Health has implemented the HIV Outbreak Response Plan, which identifies six main pillars of action:
1. Governance and coordination — Establishing a multi-sectoral task force to lead and coordinate the response to the outbreak.
2. Outbreak Investigation – Applying public health outbreak investigation principles to better understand and manage the ongoing crisis.
3. Data and surveillance systems — Enhancing data management and surveillance processes to track the rise in cases as testing expands.
4. Harm reduction and community-led prevention — Introducing high-impact prevention interventions like PrEP, needle exchange programs, and condom distribution.
5. Testing, treatment, and care scale-up — Expanding testing opportunities and ensuring that those diagnosed with HIV are connected to treatment and remain on it.
6. Resource mobilisation and awareness campaigns — Increasing public awareness and securing resources to fight the epidemic.
The plan is dynamic, continuously informed by emerging data and ongoing consultations with local communities and international partners, including UNAIDS and the US Centres for Disease Control and Prevention (CDC), which have provided technical support for the Ministry’s response efforts.
Funding and support challenges
While Fiji’s HIV response has gained support from international partners, funding for the HIV program has seen a significant decline since 2012.
Dr Tudravu noted that Government funding had decreased over the years, and international financial support has also dwindled.
In 2011, Fiji had about $5million allocated for HIV initiatives, but by 2016, that amount had plummeted to just $1.2m.
“This reduction in funding has created challenges in sustaining and expanding HIV prevention and treatment programs.
“The ministry is seeking renewed support from international partners, recognising that increased funding is crucial to scaling up the necessary interventions to address the growing crisis.”
Looking forward: Key strategies for prevention
The ministry’s National HIV Surge Strategy for 2024-2027 builds on the principles outlined in the outbreak response plan, with a specific focus on prevention.
The strategy identifies seven key objectives, including:
- Community prevention strategies — Raising awareness and promoting harm reduction methods, such as needle exchange programs and condom distribution.
- Improving HIV diagnostic services — Decentralising diagnostic services and expanding access to point-of-care testing
- Enhancing treatment and care access — Ensuring that those diagnosed with HIV can access and maintain treatment.
- Comprehensive approach to injectable drug use — Strengthening partnerships to coordinate prevention and care for individuals using intravenous drugs.
- Monitoring and research — Establishing robust systems for monitoring, evaluation, and learning to improve HIV response efforts.
The strategy emphasises that a multi-faceted approach is required to tackle HIV effectively.
With prevention, treatment, and care working in tandem, the Ministry hopes to mitigate the growing epidemic and reduce new HIV cases in the country.
Ministry’s urgent plea
As the HIV crisis in Fiji continues to evolve, the call for immediate, collective action has never been more urgent.
With HIV cases expected to increase exponentially in the next few years, it is critical that the country invests in prevention, treatment, and support services now.
Dr Lalabalvu said this was not only a health issue, but could potentially became an economic and developmental issue if we did not act now.
“The Ministry of Health cannot do this alone. We need the support of every Fijian,” Dr Lalabalavu said.
“Being diagnosed with HIV is not a ‘death sentence’.
“With adequate treatment, people living with HIV can lead a normal life — they can work, play, study and attain a degree from the university, get married, have children who don’t have HIV, run businesses and companies, and live a long, happy, and prosperous life.”
Dr Lalabalavu has called on every citizen to help break down the barriers that promote discrimination and stigma against HIV and people living with HIV.
He said more people needed to come together and act together in this serious fight against HIV.
“Talk openly and freely about how we can prevent the spread of HIV in our midst, and how we can support a colleague, a family member, a church member, or a member of our village or Vanua who has HIV to live a happy and productive life co-existing in our community.
“Then take the necessary steps to know your status and get started on treatment promptly.”