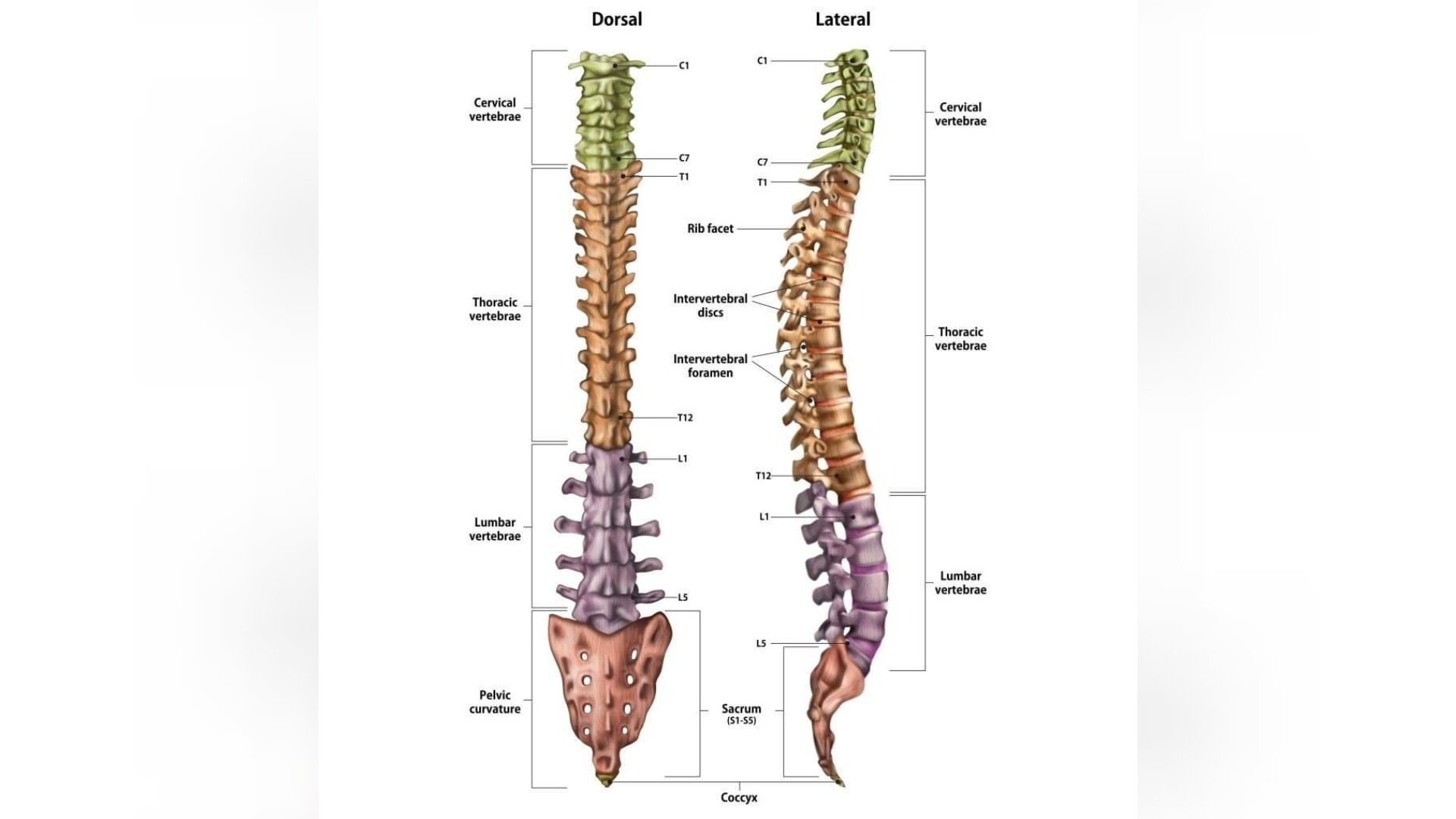
A human’s spinal cord is surrounded by a set of bones in an elongated manner called the vertebrae.
The vertebrae are divided into cervical regions that is centered around the neck consisting of seven bones, followed by thoracic vertebrae (12), then lumbar (five), sacral vertebrae are fused, comprises of five bones and last is coccyx which is also fused (four).
Each adjacent vertebra is separated by a layer of hyaline cartilage and intervertebral discs.
The intervertebral discs entail the outer annulus fibrosus that surrounds the nucleus pulposus the inner structure. Nucleus pulposus is a gelatinous substance filling the center of the intervertebral discs (IVD).
The main function of this substance is to absorb compression forces between each vertebra.
The IVD also allows smooth movement between adjacent vertebral bodies and protects the peripheral nerves that run down the spine and between the vertebrae.
The herniation of the IVD is caused by the degeneration of the annulus fibrosus.
When the outer structure becomes weakened, a part of or all the inner substance, nucleus pulposus protrudes through the degenerated outer structure resulting to herniation.
As the spine is in a constant and fully flexed position for prolonged period, it can weaken the fibrosus.
The erosion of the IVD can be caused by multitude reasons such as old age, which is the most common cause, where the nucleus pulposus becomes less hydrated and weakened.
Unhealthy lifestyle choices such as smoking and obesity can be a risk factor. Occupational causes such as drivers who drive for very long hours, athletes who play high contact sports such as rugby.
An overall bad posture during sitting, standing and even sleeping could lead to herniation of the IVD. The second most common cause of a bulging disc is trauma.
A herniation may either develop slowly over time of weeks or months or it could occur suddenly.
And out of the five regions of the vertebrae, the lumbar spine is the most common site for herniation to occur, followed by cervical spine. Since these two regions are the most flexible parts prone to wear and tear due to biomechanical forces.
The herniated disc is the combination of the nerve compression due to the bulging nucleus pulposus and the production of the chemokines resulting in inflammation. There are various types of herniation.
Such as posterolateral disc herniation which can impinge on the roots of a spinal nerve in the intervertebral foramen.
Central herniation is a lesser type of herniation however, it can lead to cauda equina syndrome. Lastly lateral disc herniation where the L4 nerve root is most often involved.
The most common clinical manifestation of IVD herniation is back pain which is also the most common cause of back pain as well.
In many cases some patients do not experience any pain in this condition. Therefore, patients need to be referred for MRI for proper diagnosis. For patients who do experience pain, describe it as a stinging or burning pain that radiates into their legs.
In more severe cases it could be associated with weakness and sensational changes. Physical therapy is the key for most patients and surgery being the last resort. A physiotherapist would first conduct a history and physical examination.
During examination attention needs to be given to weakness and sensory disturbances and their myotome and dermatomal distribution.
For example, depending on the site of herniation and specific nerve impingement, there would be specific symptoms. C5 nerve impingement would cause neck, shoulder and scapula pain, there would also be numbness in the lateral arm and weakness would be felt during movements of shoulder abduction, elbow flexion and forearm supination. Along with this, reflexes would be affected by the biceps and brachioradialis.
Another example, involving the lumbar region where nerves L2, L3 L4 are affected. It will result in pain at the back that would radiate into the anterior compartment of the thigh and medial lower leg. Along with pain, there could also be sensory loss to these areas.
Upon movements of hip flexion and adduction, there would be weakness felt along with knee extension weakness and a decrease in the patellar reflex.
Along with these specific symptoms related to the specific nerve block, there are some general symptoms that the physiotherapist would find such as patient would complain of loss of bladder and bowel control, paraspinal muscle spasm, spine or trunk deviation, tingling sensation or atrophy and weakness of the muscles.
The patient may also complain of walking difficulty. Tests would be conducted by the physiotherapist to confirm diagnosis. Such as the straight leg raise test where the patient is asked to lie in a supine position without a pillow.
The clinician would then stand at the side to be tested with one hand on the heel and the other on the thigh to ensure the knee is extended. The leg is then lifted while the knee continues to be fully extended.
This is done till the patient starts to experience tightness in the back or posterior thigh.
Reflexes are also tested both the superficial and deep tendon reflex. Sensory testing is done to look for tingling, numbness and hypoalgesia. When it comes to physical therapy management, the goal is to allow for pain control and ambulation.
It will also help to restore the lost functions in the body and even neurological deficits. Some of the exercise programs for the treatment include aerobic activity, like walking or cycling. Flexibility exercises such as yoga and stretching.
Training for proprioception, coordination and balance using medicine ball, wobble board and joint pounding. To make muscles become stronger strengthening exercises are conducted such as resistant exercise with weights and resistant bands.
Core stability exercises and ultrasound are done for soft tissue healing. Traction therapy also has positive effects on pain and disability. Hot therapies are done to increase blow flow to the targeted areas to reduce muscle spasms.
These exercises are done slowly and for a minimum of 10 minutes day for two or three times a day.
This needs to be done daily without fail for a more positive result. The exercises should be done under the guidance of a physiotherapist.
• RONEET NAND is a physiotherapist at Oceania Hospitals Pte Ltd. The views expressed in this article are the author’s and not necessarily of this newspaper.