FORCED to choose between her life and that of her unborn child, Julia Whippy found herself at the worst crossroads imaginable and at the mercy of a disease she had just been diagnosed with – lupus.
Her body had betrayed her, slowly turning on her one symptom at a time, and gradually worsening as she carried precious new life in her womb. But it ended in tragedy, with Mrs Whippy having to make the heartbreaking decision to terminate her pregnancy in 2009.
“It was one of the most painful decisions of my life,” she said.
“It was necessary – for my survival.
“It was an incredibly difficult period. I was admitted to the hospital for several months so the doctors could manage both my pregnancy and the onset of lupus, which had become quite aggressive.
“Unfortunately, due to the severity of my condition and the urgent need for strong chemotherapy medications to control the disease, I had to terminate the pregnancy.”
Lifestyle adjustments
In the wake of her diagnosis, Mrs Whippy made complete changes to her diet, focussing on foods that supported her immune system and helped reduce inflammation.
“I committed to taking my medications regularly and making my health a top priority.
“Most importantly, I worked on maintaining a strong and positive mindset. My faith played a huge role in this journey – I firmly believed, and still believe, that God will heal me from this dreadful disease in His time.”
With the support of her husband, Ben Whippy, they researched lupus in their effort to understand what they were dealing with and how to manage it.
“We looked into the types of food I could and couldn’t eat, and we educated ourselves on the symptoms, triggers, and long-term effects of the disease. Learning more about lupus helped us feel more in control and prepared for the road ahead.”
Search for a donor
In 2015, Ms Whippy travelled to India for a kidney biopsy due to complications with lupus. Following blood tests, doctors revealed her kidneys were already failing she urgently needed a kidney transplant instead of a biopsy.
“My mother was my primary caregiver and volunteered to be my donor. She underwent a series of tests to determine her compatibility.
“Unfortunately, she failed one of the most critical tests, and the doctors had to halt the donor screening process for her.
“My husband was the next to be considered as a donor. The hospital called him and informed him he would need to donate. Initially, he told the doctor we weren’t a match.”
To the couple’s surprise, they discovered the hospital could perform a specialised procedure known as an incompatible kidney transplant which allowed transplants between individuals with different blood types.
“That’s how my husband became my donor. For my body to accept his A+ kidney – since I am B+ – I had to undergo a medical procedure called plasmapheresis.
“This process involved removing my own B+ plasma from my blood and replacing it with plasma compatible with the A+ kidney. It was an intense process, but it was necessary to prevent my immune system from rejecting the transplant.”
A decade of remission
Next month will mark 10 years since the transplant took place.
“Every year is a blessing, and I’m incredibly grateful for the sacrifice, love, and support that both my husband and my mother have shown me throughout this journey.”
Mrs Whippy said she has been in remission since the transplant, and remains in a stable condition to this day.
“The transplant marked a major turning point in my journey with lupus. Before that, I endured years of uncertainty, flare-ups, and ongoing treatments.
“The procedure, though daunting, gave me a renewed sense of hope and a second chance at living a more normal and manageable life.
“Since then, I have continued to follow a disciplined treatment plan, maintain a healthy lifestyle, and attend regular medical check-ups to monitor my condition.”
Being in remission, she said, didn’t mean the end of the journey. “But it has allowed me to regain a sense of stability and peace of mind,” she said.
Hope for change
Mrs Whippy said when it came to lupus in Fiji, there were still many challenges with accessing proper healthcare and services.
“Many individuals face significant delays in proper diagnosis due to limited access to specialist care, particularly rheumatologists, as well as inadequate laboratory testing facilities.
“These delays can have serious consequences, as early detection and timely intervention are critical in managing lupus and preventing long-term organ damage.
“One of the most important changes I would like to see in hospitals and across government services in Fiji is the strengthening of diagnostic capacity for autoimmune diseases such as lupus.”
She said as the first point of contact for patients, general practitioners and nurses required more training and understanding of lupus.
“Increasing their awareness and understanding of autoimmune symptoms will help ensure patients are referred appropriately and receive the care they need without unnecessary delays.
“I would also like to see more government support and investment in awareness campaigns to educate both the public and healthcare professionals about lupus. This disease is still widely misunderstood and often overlooked.”
End the stigma
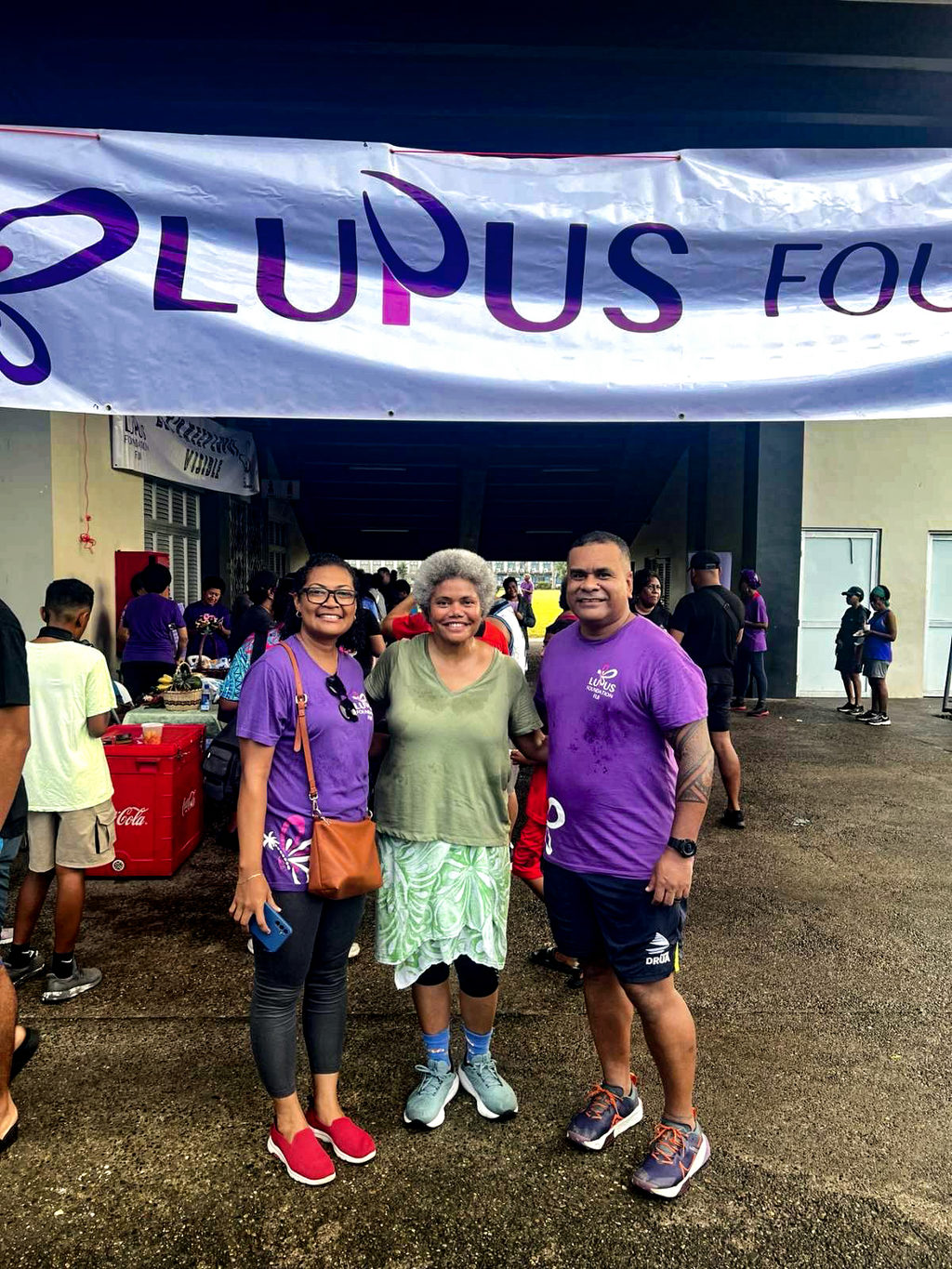
While acknowledging the work of the Lupus Foundation of Fiji, she said more government collaboration and funding was needed to broaden the reach and impact of these efforts.
“It is also essential that families of lupus patients are educated about the disease. Family understanding and support play a vital role in a patient’s emotional and physical recovery.
“When families are informed, they can provide the right kind of care, empathy, and encouragement that lupus patients need to navigate the challenges of this chronic illness.”
She said it was tragic to hear of young people dying as a result of the misconceptions of lupus.
“It’s incredibly upsetting that such cases still happen, where a lack of awareness leads to avoidable tragedy. These misconceptions must be addressed.
“It’s time to put an end to the stigma and misinformation surrounding lupus and other autoimmune diseases.
“This is not witchcraft. It is a medical condition that can be managed with the right treatment and support.”