AS I write this op-ed, we mourn the passing of a true champion of a Needle and Syringe Programme in Fiji, permanent secretary for Health and Medical Services, Dr Jemesa Tudravu, on December 27, 2025. This op-ed is dedicated to Dr Tudravu.
Fiji is at an important moment in its response to HIV. Around the world, countries occasionally face periods where HIV infections rise, often when prevention efforts have not yet adapted to changing realities. What matters most is how we respond, and whether we choose approaches that are proven, compassionate, and focused on protecting the health of everyone.
One such approach is the introduction of Needle and Syringe Programs, commonly known as NSPs. These programs have been used for decades in many countries and communities. They are well understood in public health, but they are sometimes misunderstood by the broader public. This is why it is
important to explain clearly what NSPs are, how they work, and why they matter for Fiji.
What is a Needle and Syringe Program?
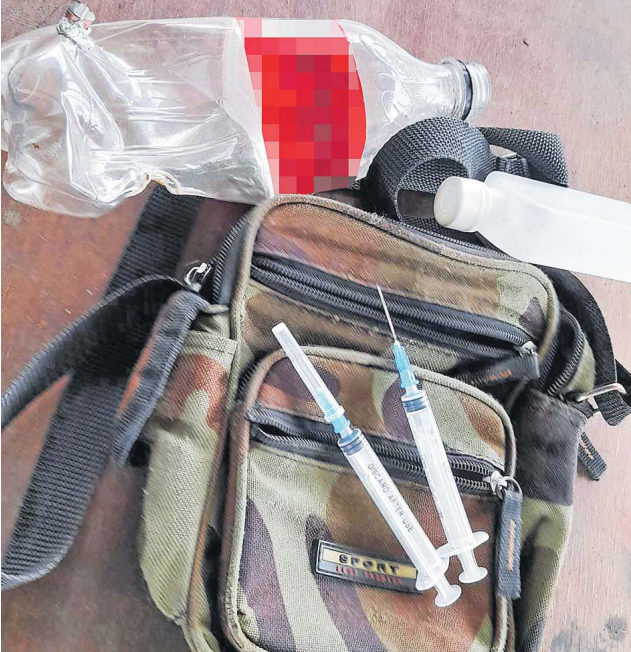
A NEEDLE and Syringe Program (NSP ) – also sometimes refers to a needle exchange program – is a public health intervention designed to reduce health harms associated with injecting drug use, both for individuals and for the wider community. An NSP provides free, sterile injecting equipment (needles, syringes, and often related items) to people who inject drugs, and safely disposes of used equipment. The primary goal is harm reduction, not promoting or condoning drug use.
But doesn’t this promote drug use?
NSPs are a public health measure designed to reduce the spread of HIV and other blood-borne infections by ensuring access to sterile injecting equipment and safe disposal. They are not about encouraging drug use. They are about preventing illness, protecting families and communities, and creating opportunities for people to connect with health and support services.
International experience is clear. Countries such as Australia, New Zealand, Portugal, and parts of Europe and Asia have used NSPs as part of comprehensive HIV prevention strategies. These countries have seen significant reductions in HIV and hepatitis transmission, without increases in drug use or crime. In many settings, NSPs have also helped people access HIV testing, treatment, counselling, and, where needed, pathways to rehabilitation and recovery. NSP centres are a place where drug users can be reached, and optional counselling and other services can be provided. In my home country Germany, overall evidence indicates that the country’s harm-reduction approach, including NSPs alongside opioid substitution treatment, has contributed to a marked decrease in new HIV infections among people who inject drugs over recent years by reducing unsafe needle sharing and other risk behaviours. In a Berlin prison NSP saw syringe sharing drop from about 71 per cent to around 11 per cent after implementation, with sharing rates remaining very low thereafter, which strongly lowers the risk of HIV/HBV/HCV transmission among inmates who inject drugs.
Is my community and neighbourhood safe in the vicinity of NSP centres?
Another common concern is whether NSPs affect community safety. In practice, NSPs often improve safety. By reducing needle sharing and supporting safe disposal, these programs lower the risk of accidental needle-stick injuries to the public, sanitation workers, and law enforcement officers. They also reduce long-term pressure on health systems by preventing infections that require lifelong care.
The true benefits:
At their heart, NSPs recognise a simple reality. Public health challenges are best addressed through care, evidence, and inclusion. When people feel safe to access services, everyone benefits. NSPs help reduce stigma, build trust, and ensure that prevention reaches those most at risk, which ultimately protects the wider community.
In Fiji, we often speak of veiqaravi (caring for one another), veilomani (compassion), and talanoa (open and respectful dialogue). NSPs reflect these values by focusing on care, prevention, and shared responsibility for the wellbeing of our communities, or na bula vinaka ni vanua.
In Fiji, progress toward NSPs has been careful, inclusive, and nationally led. The Minister for Health and Medical Services, Dr Atonio Lalabalavu, supported by the later permanent secretary Dr Tudravu, have been closely involved and has shown strong leadership and commitment to advancing this work as part of Fiji’s HIV outbreak response. NSPs are embedded within the National HIV Surge Strategy and the Fiji Narcotics Strategy and are being developed alongside clear safeguards, strong governance, and appropriate legal frameworks.
What type of support have the United Nations provided?
The United Nations has been actively supporting Fiji throughout this process. UNAIDS, WHO, UNFPA, UNDP, UNICEF, ILO and other partners have worked alongside the Ministry of Health and Medical Services to share global evidence, provide technical support, and facilitate open dialogue. This has included national consultations, engagement with law enforcement and faith-based organisations, peer educator training, and a national implementation workshop bringing together government, communities, and technical experts.
Community leadership has been central to this journey. Peer educators and community networks play a vital role in reaching people with accurate information, promoting safer practices, and linking individuals to care. Around the world, responses that place communities at the centre have proven to be the most effective and sustainable.
The role of the United Nations is to support nationally owned solutions that are grounded in evidence, human rights, and public health. NSPs are not a standalone intervention. They work best when combined with HIV testing, treatment, prevention tools such as PrEP, mental health support, and strong referral systems. Together, these approaches form a comprehensive and balanced response.
Why now?
Some may wonder whether NSPs are the right step for Fiji right now. Global experience suggests that early, evidence-based action saves lives and resources. Preventing HIV infections today avoids lifelong health impacts and health costs tomorrow, for individuals, families, and the health system as a whole.
Ending HIV transmission is an achievable goal. Countries that have invested in prevention, community engagement, and leadership have already demonstrated what is possible. Fiji has the opportunity to build on global best practices while shaping an approach that reflects its own values, culture, and strengths.
By choosing evidence, care, and collective responsibility, Fiji can protect its communities and its future. With continued leadership, partnership, and understanding, ending HIV transmission is within reach. Together, we can make it happen.
Q&A: Understanding Needle and Syringe Programs (NSPs)
What exactly is a Needle and Syringe Program?
An NSP provides access to sterile needles and syringes, along with safe disposal, health information, and referrals to services. Its purpose is to prevent the spread of HIV and other blood-borne infections and to protect public health.
Do NSPs encourage drug use?
No. Decades of evidence from countries including Australia and New Zealand show that NSPs do not increase drug use. They reduce harm and often help people connect with health services, counselling, and treatment options.
Why not focus only on stopping drug use altogether?
Prevention and recovery services are important, but they do not reach everyone immediately. NSPs protect lives now, while longer-term support and recovery pathways continue. This is about saving lives today while supporting healthier futures.
Are NSPs safe for communities?
Yes. NSPs reduce needle sharing and unsafe disposal, which protects the public, waste workers, and police from accidental injuries. Communities often become safer, not less safe.
Are NSPs legal in Fiji?
NSPs in Fiji are being developed carefully, with appropriate laws, regulations, and safeguards to ensure they are safe, well governed, and aligned with national priorities.
Who is involved in delivering NSPs?
NSPs are delivered through the health system, working closely with trained peer educators and community organisations. This ensures services are trusted, accessible, and culturally appropriate.
Why is the UN supporting NSPs in Fiji?
The United Nations supports Fiji by sharing global evidence, best practices, technical expertise, and lessons from other countries, while respecting national leadership and decision-making. The goal is to support Fiji to protect its people and end HIV transmission.
How does this help end HIV transmission?
By preventing new infections, linking people to testing and treatment, and strengthening community trust, NSPs help stop HIV from spreading further. Combined with other prevention and treatment efforts, they move Fiji closer to ending HIV transmission.